What is Twin to Twin Transfusion Syndrome?
TWIN TO TWIN TRANSFUSION SYNDROME - TTTS
Twin to Twin Transfusion Syndrome, commonly referred to as TTTS, is a disease of the placenta affecting identical twins (or higher order multiples) who share that placenta. In simple terms, there is an uneven flow of blood and nutrients between the twins, resulting in one twin, (the “Recipient”), receiving too much blood – which causes excessive strain on the heart – and the other twin, (“the Donor”), with too little blood – resulting in anaemia and low body weight.
The Recipient twin will also be surrounded by excessive amniotic fluid, and the Donor twin very little. One of the early signs of TTTS can be a sudden increase in size of the mother due to the large amounts of amniotic fluid surrounding the Recipient twin. Ultrasounds are crucial in diagnosis of TTTS, with the key factors being significant differences in size of the babies, the size of the Donor twin’s bladder, and the amount of amniotic fluid surrounding each twin.
TTTS can occur at any time during pregnancy. At its most severe, it occurs before 20 weeks, usually resulting in a high mortality rate for one or both twins. TTTS can occur as late as during delivery of the babies, or even between the birth of the first and second twin. Where TTTS has been present for some time, it is often the Recipient twin who struggles more after the birth, having worked so hard pumping all the extra blood.
Depending on when the diagnosis of TTTS occurs, and the extent to which it is affecting the babies, the treatment varies. It is possible to stop the transfusion of blood via laser treatment to seal off the blood vessels, however this treatment is relatively new in Australia. Other treatments treat the symptoms rather than the cause, such as reducing the excess amniotic fluid from the recipient twin.
STAGES OF TTTS
1
2
The bladder of the Donor twin is not visible or it does not fill with urine during an ultrasound exam.
3
Imbalance of blood flow starts to affect the heart function in one or both babies. This is seen in abnormal blood flow in the umbilical cords or hearts of the twins.
4
The imbalance of blood flow causes signs of heart failure in one of the twins.
5
One or both of the twins has passed away from severe TTTS.
DURING PREGNANCY
Symptoms
During pregnancy, mothers should be aware of and look out for the following symptoms:
- tightness in the abdomen or unusually rapid expansion of abdomen
- pressure on the stomach
- breathlessness
- rapid weight gain
How is TTTS diagnosed?
During pregnancies of twins (or higher order multiples) who share a placenta, it is recommended that screening ultrasounds be performed at least every fortnight from 16 weeks until delivery. If signs of TTTS develop, such as a varying amniotic fluid levels or growth differences, ultrasounds should be performed more frequently to determine if TTTS is progressing. Treatment options depend on the stage of TTTS, and range from observation to placental laser surgery.
TREATMENT OPTIONS
No treatment
Leaving severe TTTS untreated is associated with a high loss rate of both babies due to premature labor, premature rupture of membranes, and/or early delivery or loss can occur before birth from the direct effects of TTTS.
Observation
Stage 1 cases may not require intervention, but it is important to monitor the twins’ progress frequently and closely, to rule out progression.
Laser surgery – Placental ablation
Placental ablation is the only treatment that targets the cause of the TTTS and is generally performed between 16-24 weeks. Surgeons insert a thin telescope into the uterus and use a laser to block the blood vessels connected between the two foetuses. This allows each twin to develop independently.
While the maternal risk of fetal surgery is minimal, both minor and major complications can occur.
Amnioreduction
This procedure removes the excess fluid from around the Recipient twin, reducing amniotic pressure and reducing the risk of preterm labor. This is usually performed with placental ablation surgery.
Amnioreduction does not treat the cause of TTTS and may have to be repeated, as the fluid is likely to accumulate again. With each procedure, the risk of bleeding, infection and injury to the membranes increases. Amnioreduction is mostly used when TTTS is not severe enough to threaten the fetuses, as a way to offer comfort to the mother when day-to-day activities and even breathing become a problem.
TTTS RELATED COMPLICATIONS
Selective Intrauterine Growth Restriction (SIGUR)
When identical twins share a single placenta, they may not share it equally and one twin may fail to grow properly—referred to as growth restriction. The twin with growth restriction will usually be significantly smaller than its co-twin and we call this selective fetal growth restriction.
If the growth restriction is particularly severe it can pose significant risks for both twins. In pregnancies with TTTS, selective fetal growth restriction can occur at the same time, adding extra risk to the pregnancy and making management even more complicated.
TAPS
Twin Anaemia Polycythainia Sequence, or TAPS, occurs when one twin has a low blood count (anaemia) and the other twin a high blood count (polycythaemia). It can occur on its own or may happen after laser therapy for TTTS. Some cases of TAPS do not require specific treatment other than regular ultrasound monitoring.
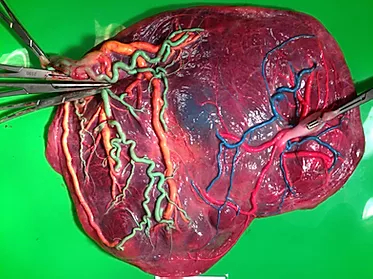
TTTS MONOCHORIONIC PLACENTA PICTURES
Amanda Walliss
TTTS Stage 3 diagnosed at 28+2, morning of 28+3 had progressed to Stage 4. Laser surgery and amnio reduction same day as Stage 4 diagnosis. Twins Ava and Cleo born by c-section at 34+6 on 27 November 2015, both did amazing, 2 weeks in NICU/ special care with no long term health impacts for either.

Stephanie Ernst
TTTS stage 1 diagnosed at 24 weeks, spontaneously resolved over the next few weeks. TAPS diagnosed shortly after. No laser surgery, completely spontaneous TAPS. Twins Emilie and Mathilde born 31+1 weeks.